Bone tissue is the most important tissue in our body. It performs many functions. Bone tissue in histology is referred to as a variety of skeletal connective tissue, which also includes cartilage tissue. Cells of skeletal connective tissues, including bone, develop from the mesenchyme.
Skeletal connective tissues
Skeletal connective tissues perform many functions:
- Bones are the backbone of the whole organism. The skeleton allows a person, consisting entirely of soft tissues, to feel confident in space.
- Thanks to the skeleton we can move. Muscles are attached to bones, which in turn form levers of movement that allow you to perform any action.
- The depot of many minerals is located in the bone tissue. Bone tissue is involved in the metabolism of phosphate and calcium.
- Hematopoiesis occurs in the bones, namely in the red bone marrow.
The functions of bone tissue in histology are defined as coinciding with the functions of allskeletal connective tissues, but this tissue has a number of unique properties.
The main feature and difference between bone tissue and other connective tissue is its high content of minerals, which is 70%. This explains the strength of the bones, because the intercellular substance of the bone connective tissue is in a solid state.
Bone tissues. The chemical composition of bone tissue

Bone tissue must begin with the study of its chemical composition. This will allow you to understand its special properties. The content of organic substances in the tissue is from 10 to 20%. Water contains from 6% to 20%, minerals, as mentioned above, most of all - up to 70%. The main elements of the mineral substance of the bone are calcium phosphate and hydroxyapatites. Also high in mineral s alts.
The combination of organic and inorganic substances of bone tissue explains the strength, elasticity of bones, their ability to withstand heavy loads. At the same time, too high a mineral content makes the bones significantly brittle.
The intercellular substance is formed by 95% type I collagen. Organic matter accumulates on protein fibers. Phosphoproteins contribute to the accumulation of calcium ions in the bones. Proteoglycans promote the binding of collagen to mineral compounds, the formation of which, in turn, is assisted by alkaline phosphatase and osteonectin, which stimulates further growth of inorganic crystals.
Cell components
Bone cells inHistology is divided into three types: osteoblasts, osteocytes and osteoclasts. Cellular components interact with each other, forming an integral system.
Osteoblasts
Osteoblasts are cubic, oval-shaped cells with an eccentrically located nucleus. The size of such cells is approximately 15-20 microns. Organelles are well developed, granular EPS and the Golgi complex are expressed, which can explain the active synthesis of exported proteins. In histology, on a bone tissue preparation, the cytoplasm of cells stains basophilically.
Osteoblasts are localized on the surface of the bone beams in the emerging bone, where they remain in mature bones in the spongy substance. In formed bones, osteoblasts can be found in the periosteum, in the endosteum covering the medullary canal, in the perivascular space of osteons.
Osteoblasts are involved in osteogenesis. Due to the active synthesis and export of proteins, a bone matrix is formed. Thanks to alkaline phosphatase, which is active in the cell, there is an accumulation of minerals. Do not forget that osteoblasts are the precursors of osteocytes. Osteoblasts secrete matrix vesicles, the contents of which trigger the formation of crystals from minerals in the bone matrix.
Osteoblasts are divided into active and resting. Active ones participate in osteogenesis and produce matrix components. Resting osteoblasts with an endosteal membrane protect bone from osteoclasts. Resting osteoblasts can be activated whenbone adjustment.
Osteocytes
Osteocytes are mature, well-differentiated cells of bone tissue, located one at a time in gaps, also called bone cavities. Oval-shaped cells with numerous processes. The size of osteocytes is approximately 30 microns in length and up to 12 in width. The core is elongated, located in the center. Chromatin is condensed and forms large clumps. Organelles are poorly developed, which may explain the low synthetic activity of osteocytes. Cells are connected to each other by processes through cell contacts of nexuses, forming syncytium. Through the processes, there is an exchange of substances between bone tissue and blood vessels.
Osteoclasts
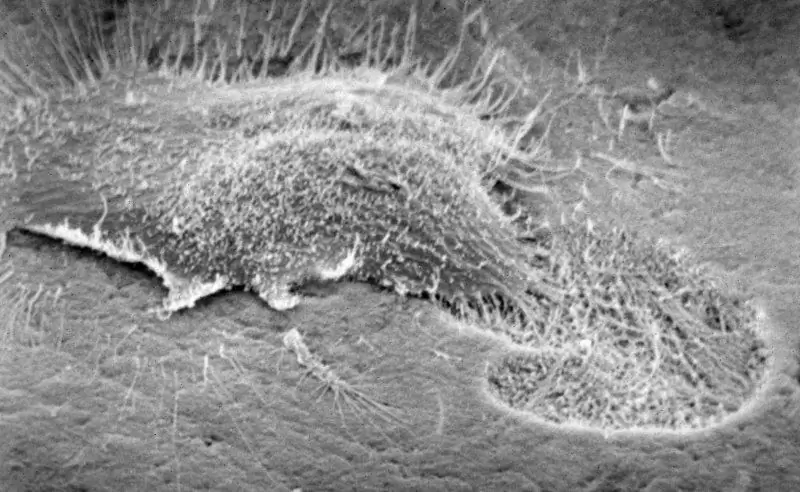
Osteoclasts, unlike osteoblasts and osteocytes, originate from blood cells. Osteocytes are formed by the fusion of several promonocytes, so some authors do not consider them cells and classify them as symplasts.
By structure, osteoclasts are large, slightly elongated cells. Cell size can vary from 60 to 100 µm. The cytoplasm can stain both oxyphilly and basophilically, it all depends on the age of the cells.
There are several zones in a cage:
- Basal, containing the main organelles and nuclei.
- Ruffled border of microvilli penetrating the bone.
- Vesicular zone containing bone-degrading enzymes.
- Light-colored adherence zone to promote cell fixation.
- Zoneresorption
Osteoclasts destroy bone tissue, are involved in bone remodeling. The destruction of the bone substance, or, in other words, resorption, is an important stage of restructuring, followed by the formation of a new substance with the help of osteoblasts. Localization of osteoclasts coincides with the presence of osteoblasts, in depressions on the surfaces of bone beams, in the endosteum and periosteum.
Periosteum
The periosteum is made up of osteoblasts, osteoclasts, and osteogenic cells that are involved in bone growth and repair. The periosteum is rich in blood vessels, the branches of which wrap around the bone, penetrating into its substance.
In histology, the classification of bone tissue is not very extensive. Fabrics are divided into coarse fiber and lamellar.
Coarse fibrous bone tissue
Coarse fibrous bone tissue occurs mainly in a child before birth. In an adult, it remains in the sutures of the skull, in the dental alveoli, in the inner ear, in the places where the tendons are attached to the bones. Coarse-fibrous bone tissue in histology is determined by the predecessor of lamellar.
Tissue consists of chaotically arranged thick bundles of collagen fibers, which are located in a matrix consisting of inorganic substances. In the intercellular substance there are also blood vessels, which are rather poorly developed. Osteocytes are located in the intercellular substance in the systems of lacunae and canals.
Lamellar bone tissue
All bones of the adult body, with the exception of the places of attachment of tendons and areas of cranial sutures, consist of lamellar boneconnective tissue.
Unlike coarse fibrous bone tissue, all components of lamellar tissue are structured and form bone plates. Collagen fibers within one plate have one direction.
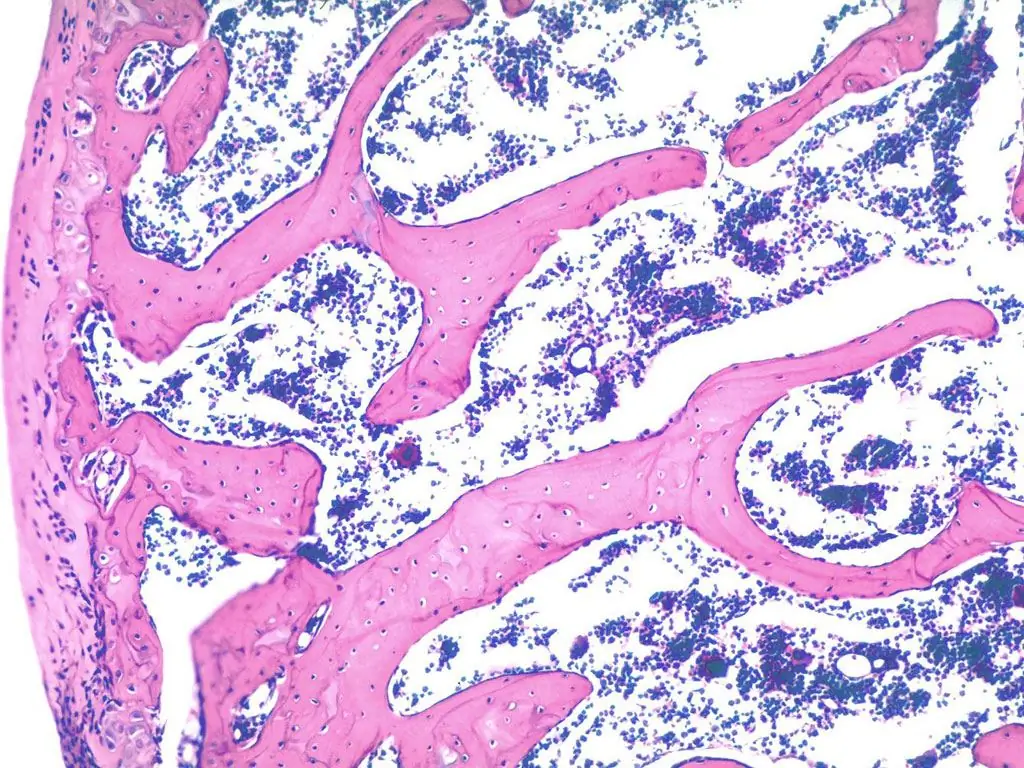
There are two varieties of lamellar bone tissue in histology - spongy and compact.
Spongy matter
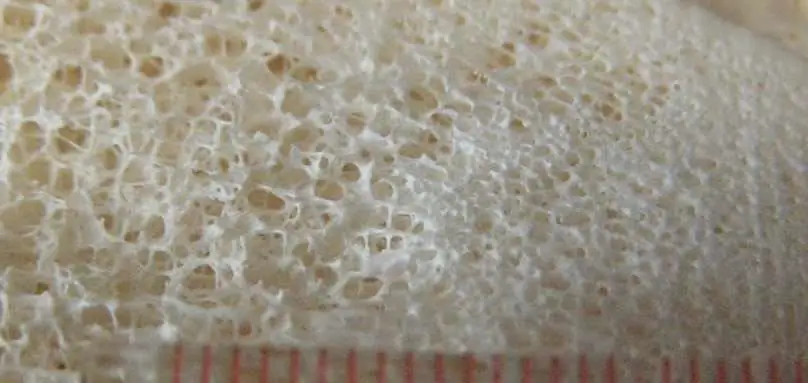
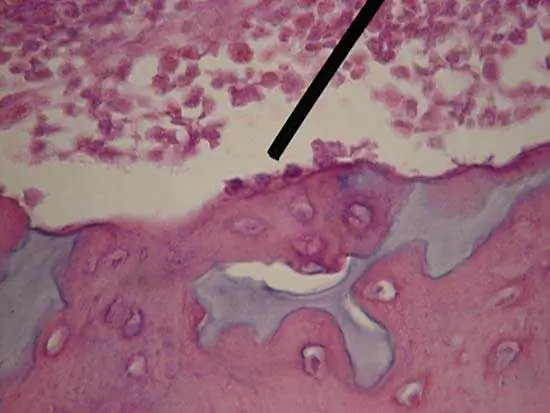
In the spongy substance, the plates are combined into trabeculae, the structural units of the substance. Arcuate plates lie parallel to each other, forming avascular bone beams. The plates are oriented along the direction of the trabeculae themselves.
Trabeculae are connected to each other at different angles, forming a three-dimensional structure. Bone cells are located in the gaps between the bone beams, which makes this substance porous, explaining the name of the tissue. The cells contain red bone marrow and blood vessels that feed the bone.
Spongy substance is located in the inner part of the flat and spongy bones, in the epiphyses and inner layers of the tubular diaphysis.
Compact bone matter
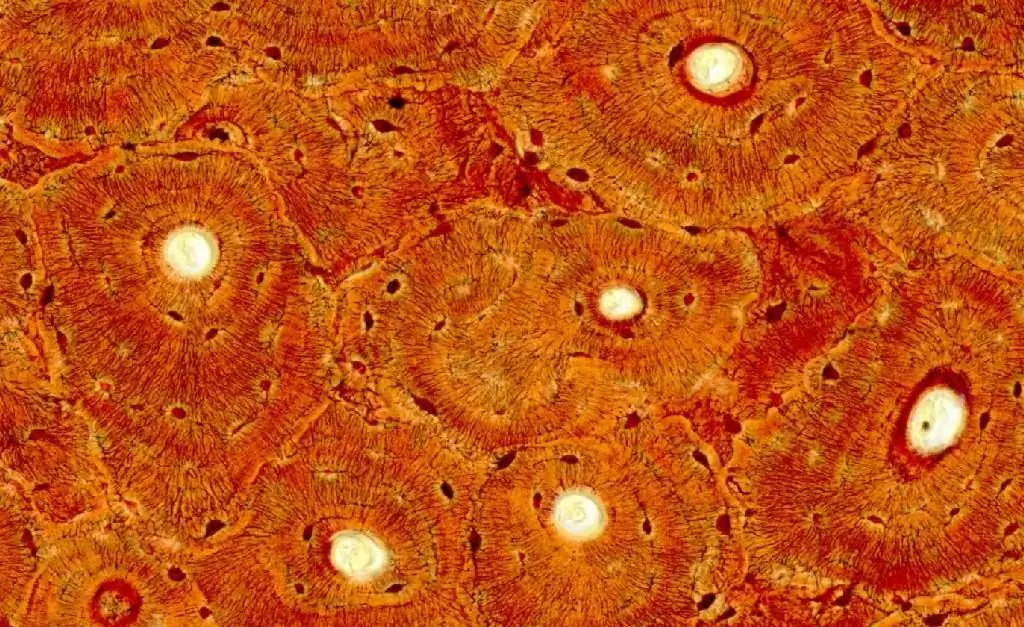
The histology of lamellar bone tissue should be well studied, because it is this type of bone tissue that is the most complex and contains many different elements.
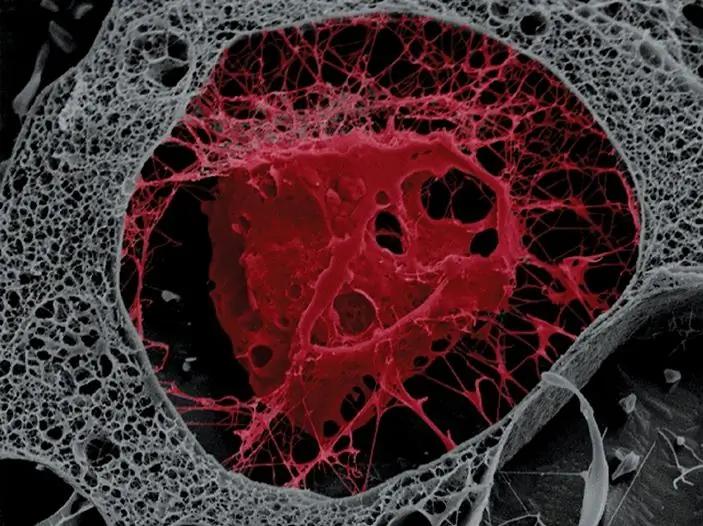
Bone plates in a compact substance are arranged in a circle, they are inserted into each other, forming a dense pile, where there are practically no gaps. The structural unit is the osteon, formedbone plates. Records can be divided into several types.
- Outer general plates. They are located directly under the periosteum, encircling the entire bone. In spongy and flat bones, compact substance can only be expressed by such plates.
- Osteon plates. This type of plate forms osteons, concentric plates lying around the vessels. Osteon is the main element of the compact substance of the diaphyses in tubular bones.
- Inset plates, which are the remains of decaying plates.
- Internal general lamellae surround the medullary canal with yellow marrow.
The compact substance is localized in the surface layer of flat and spongy bones, in the diaphysis and superficial layers of the epiphysis of tubular bones.
The bone is covered with periosteum, which contains cambial cells, thanks to which the bone grows in thickness. The periosteum also contains osteoblasts and osteoclasts.
Under the periosteum lies a layer of outer general plates.
In the very center of the tubular bone is the medullary cavity, covered with endosteum. Endost is covered with internal general plates, enclosing it in a ring. Trabeculae of spongy substance may adjoin the medullary cavity, so in some places the plates may become less pronounced.
Between the outer and inner layers of the general plates is the osteon layer of the bone. At the center of each osteon is a Haversian canal with a blood vessel. Haversian channels communicate with each other by transverse Volkmann channels. The space between the plates and the vessel is called perivascular, the vessel is covered with loose connective tissue, and the perivascular space contains cells similar to those of the periosteum. The channel is surrounded by layers of osteon plates. In turn, the osteons are separated from each other by a resorption line, which is often called the cleavage. Also between the osteons are intercalated plates, which are the residual material of the osteons.
Bone gaps with osteocytes enclosed in them are located between the osteon plates. The processes of osteocytes form tubules, through which nutrients are transported to the bones perpendicular to the plates.
Collagen fibers make it possible to see bone channels and cavities under a microscope, as areas lined with collagen are stained brown.
In histology on the preparation, lamellar bone tissue is stained according to Schmorl.
Osteogenesis
Osteogenesis is either direct or indirect. Direct development is carried out from the mesenchyme, from the cells of the connective tissue. Indirect - from cartilage cells. In histology, direct osteogenesis of bone tissue is considered before indirect, because it is a simpler and more ancient mechanism.
Direct Osteogenesis
The bones of the skull, small bones of the hand and other flat bones develop from the connective tissue. In the formation of bones in this way, four stages can be distinguished
- Formation of the skeletal primordium. In the first month, stromal stem cells enter the mesenchyme from somites. There is a multiplication of cells, enrichment of the tissue with vessels. Under the influence of growth factors, cells form clusters of up to 50 pieces. Cells secrete proteins, multiply and grow. In stem stromal cells, the process of differentiation starts, they turn into osteogenic progenitor cells.
- Osteoid stage. In osteogenic cells, protein synthesis and glycogen accumulation occur, the organelles become larger, they function more actively. Osteogenic cells synthesize collagen and other proteins, such as bone morphogenetic protein. Over time, cells begin to multiply less frequently and differentiate into osteoblasts. Osteoblasts are involved in the formation of the intercellular substance, poor in minerals and rich in organic matter, osteoid. It is at this stage that osteocytes and osteoclasts appear.
- Osteoid mineralization. Osteoblasts are also involved in this process. Alkaline phosphatase begins to work in them, the activity of which contributes to the accumulation of minerals. Matrix vesicles filled with the protein osteocalcin and calcium phosphate appear in the cytoplasm. Minerals adhere to collagen due to osteocalcin. Trabeculae increase and, connecting with each other, form a network where mesenchyme and vessels still remain. The resulting tissue is called primary membranous tissue. The bone tissue is coarse-fibred, forming the primary cancellous bone. At this stage, the periosteum is formed from the mesenchyme. Cells appear near the blood vessels of the periosteum, which will then participate in the growth and regeneration of the bone.
- The formation of bone plates. At this stage, there isreplacement of primary membranous bone tissue with lamellar. Osteons begin to fill the gaps between the trabeculae. Osteoclasts enter the bone from blood vessels and form cavities in it. It is osteoclasts that create a cavity for the bone marrow, affect the shape of the bone.
Indirect Osteogenesis
Indirect osteogenesis occurs during the development of tubular and spongy bones. To understand all the mechanisms of osteogenesis, you need to be well versed in the histology of cartilage and bone connective tissues.
The whole process can be divided into three steps:
- Formation of cartilage model. In the diaphysis, chondrocytes become deficient in nutrients and become blistered. The released matrix vesicles lead to calcification of the cartilaginous tissue. In histology, cartilage and bone tissue are interconnected. They start replacing each other. The perichondrium becomes the periosteum. Chondrogenic cells become osteogenic, which in turn become osteoblasts.
- Formation of primary cancellous bone. Rough fibrous connective tissue appears in place of the cartilaginous model. A perichondral bone ring, a bony cuff, is also formed, where osteoblasts form trabeculae right at the site of the diaphysis. Due to the appearance of a bone cuff, cartilage nutrition becomes impossible, and chondrocytes begin to die. Cartilage and bone tissue in histology are very interconnected. Following the death of chondrocytes, osteoclasts form channels from the periphery of the bone to the depth of the diaphysis, along which osteoblasts, osteogenic cells, and blood vessels move. Endochondral ossification begins, eventually turning into epiphyseal.
- Rebuilding the fabric. Primary coarse fibrous tissue gradually turns into lamellar.
Growth and development of bone tissue
Bone growth in humans goes up to 20 years. The bone grows in width due to the periosteum, in length due to the metaepiphyseal growth plate. In the metaepiphyseal plate, one can distinguish the zone of resting cartilage, the zone of columnar cartilage, the zone of vesicular cartilage and the zone of calcified cartilage.
Many factors influence bone growth and development. These can be factors of the internal environment, environmental factors, lack or excess of certain substances.
Growth is accompanied by the resorption of old tissue and its replacement by a new young one. In childhood, bones grow very actively.
Bone growth is influenced by many hormones. For example, somatotropin stimulates bone growth, but with its excess, acromegaly can occur, with a deficiency - dwarfism. Insulin is essential for the proper development of osteogenic and stem stromal cells. Sex hormones also affect bone growth. Their increased content at an early age can lead to shortening of the bones due to early ossification of the metaepiphyseal plate. Their reduced content in adulthood can lead to osteoporosis, increase bone fragility. The thyroid hormone calcitonin leads to the activation of osteoblasts, parathyrin increases the number of osteoclasts. Thyroxine affects the centers of ossification, hormones of the adrenal glands - the regeneration processes.
Bone growth hasinfluence also some vitamins. Vitamin C promotes collagen synthesis. With hypovitaminosis, a slowdown in bone tissue regeneration can be observed, histology in such processes can help to find out the causes of the disease. Vitamin A accelerates osteogenesis, you should be careful, because with hypervitaminosis there is a narrowing of the bone cavities. Vitamin D helps the body absorb calcium, with beriberi, bones are bent. At the same time, the formed plastic bone tissue in histology is accompanied by the term osteomalacia, and such symptoms are also characteristic of rickets in children.
Reshaping the bone
In the process of restructuring, coarse fibrous connective tissue is replaced with lamellar tissue, bone substance is renewed, and mineral content is regulated. On average, 8% of the bone substance is renewed per year, and the spongy tissue is renewed 5 times more intensively than the lamellar one. In the histology of bone tissue, special attention is paid to the mechanisms of bone remodeling.
Restructuring includes resorption, tissue destruction and osteogenesis. With age, resorption may predominate. This explains osteoporosis in the elderly.
The process of restructuring consists of four stages: activation, resorption, reversion and formation.
Regeneration of bone tissue in histology is considered as a kind of bone remodeling. This process is very important, but most importantly, knowing the factors that affect the regeneration process, we can accelerate it, which is very important in case of bone fractures.
Knowledge of histology, human bone tissue is useful for both doctors and ordinary people. Understanding some mechanisms can help even in everyday things, for example, in the treatment of fractures, in the prevention of injuries. The structure of bone tissue in histology is well studied. But still, the bone tissue is far from being fully explored.






